Opportunity for Nerve Imaging
Unintended Nerve Injury is a Serious Condition with a High Unmet Need
Surgery plays a prominent role as first line treatment across many medical conditions. The ultimate goal of surgery is to repair or remove damaged and/or diseased tissue while preserving vital structures, such as nerves. Even with advanced surgical techniques, such as the increasing adoption of minimally invasive access and nerve-sparing techniques, iatrogenic nerve injury (i.e. injury caused by medical examination or treatment) remains a leading cause of morbidity across many common surgical procedures. An accurate estimate of the overall incidence of iatrogenic nerve injury in surgeries is unknown due to the heterogeneity in reporting; however, available estimates range between 1.5% - 15%. 1 2
As the rate of surgical procedures continues to increase annually, the risk of iatrogenic nerve injury also increases. Approximately 100 million surgical procedures, both inpatient and ambulatory, are performed in the US each year.3 To quantify the size of the unmet need, assuming an average incidence rate for iatrogenic nerve injury of 10%, greater than 10 million patients in the US are at risk annually.
Iatrogenic nerve injury is a leading cause of morbidity associated with many common surgical procedures including prostatectomy, herniorrhaphy, coronary artery bypass graft, thyroidectomy, lumpectomy, mastectomy, hip and knee replacement, vascular bypass, colorectal surgery and gynecologic surgery amongst others.4 5 In a retrospective study of >380,000 cases at a single institution over 10 years, surgical procedures associated with the highest incidence of nerve injury included Orthopedic (21%), General Surgery (18%), Urology (13%), Neurosurgical (8.9%) and Cardiac (7.1%).6
Complications arising from these iatrogenic nerve injuries are often permanent and may result in:
- loss of function and/or sensation in limbs and organs
- muscle atrophy
- persistent numbness and pain
- chronic neuropathy
- reduced quality of life
- disability
- paralysis
Did you know?
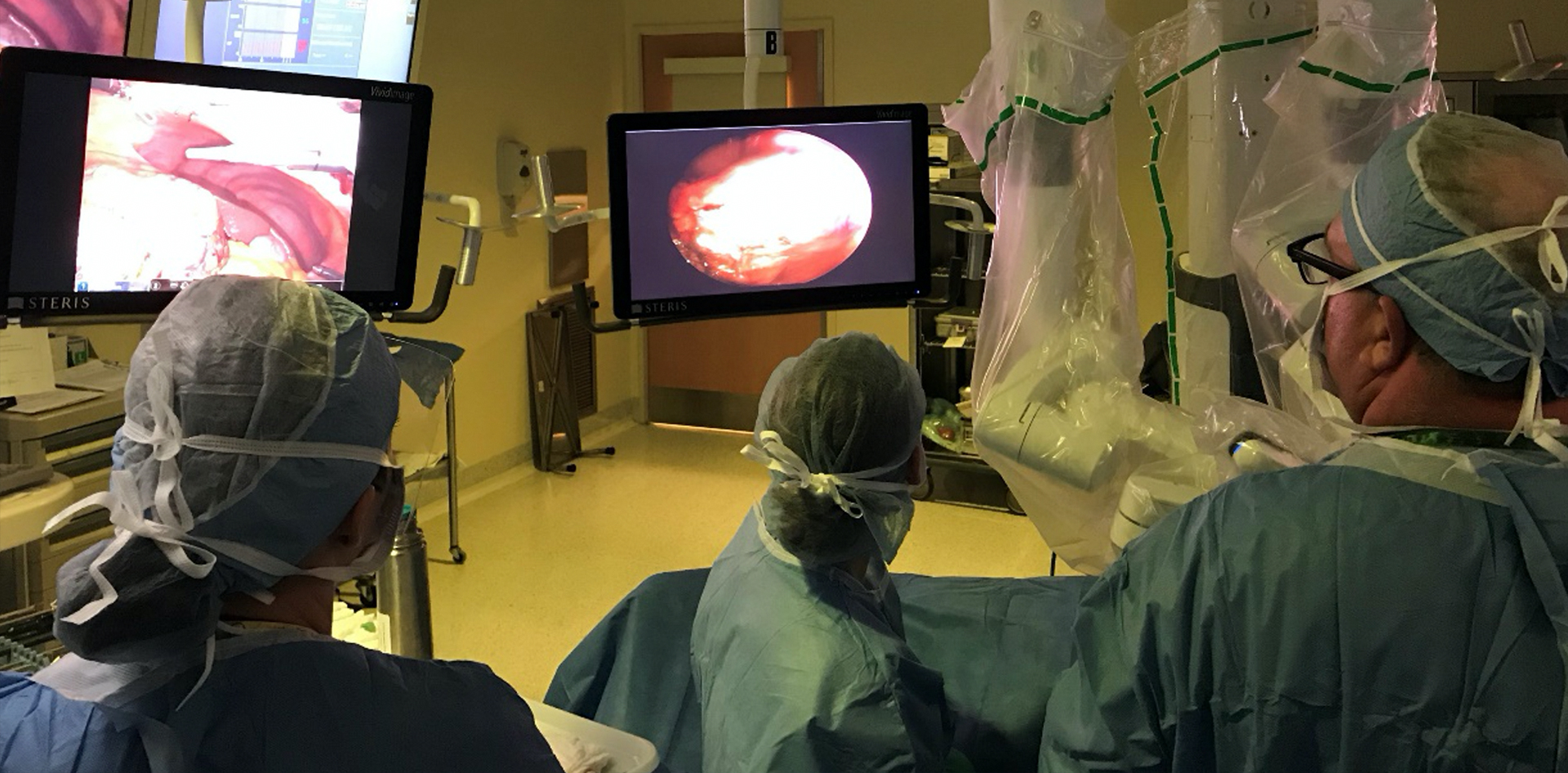
In the field of urology, urinary and sexual dysfunction are common after radical prostatectomy and cystoprostatectomy as a result of nerve damage. The cavernous nerves in the neurovascular bundle are often difficult to visualize during surgery not only because of anatomical variations in their location, but also their intricacy since they appear as more of a network of fine structures rather than a distinct anatomical structure. Even with the advent of nerve sparing techniques, which rely primarily upon anatomical landmark identification, erectile dysfunction occurs in 50 – 87% of the cases. It is estimated that 60% of men continue to experience erectile dysfunction 18 months post-operatively, only ~ 20% report erections strong enough for intercourse 5 years after surgery and a modest 20% of men return to pre-operative erectile function within the first year following the procedure.7
References:
1. Anesti K, Caine P Plast Aesthet Res 2015;2:309-310
2. Vecchio, Michele & Andrea, Santamato & Fortunato, Genovese & Malaguarnera, Giulia & Catania, Vito & Latteri, Saverio. (2018). Iatrogenic nerve lesion following laparoscopic surgery. A case report. Annals of Medicine and Surgery. 28. 10.1016/j.amsu.2018.02.002.
3. NQF-Endorsed Measures for Surgical Procedures, 2015-2017 FINAL REPORT APRIL 20, 2017
4. Cotero VE, et al. Improved Intraoperative Visualization of Nerves through a Myelin-Binding Fluorophore and Dual-Mode Laparoscopic Imaging. 2015 PLoS ONE 10(6):e0130276.
5. Walsh EM, et al. Fluorescence Imaging of Nerves During Surgery, 2019 AnnSurg, 270:69-76.
6. Welch MB, Perioperative peripheral nerve injuries: A retrospective study of 380,680 cases during a 10-year period at a single institution. Anesthesiology 2009;111:490-7.
7. Whelan, Patrick et al. “Erectile dysfunction in robotic radical prostatectomy: Outcomes and management.” IJU vol. 30,4 (2014): 434-42.

